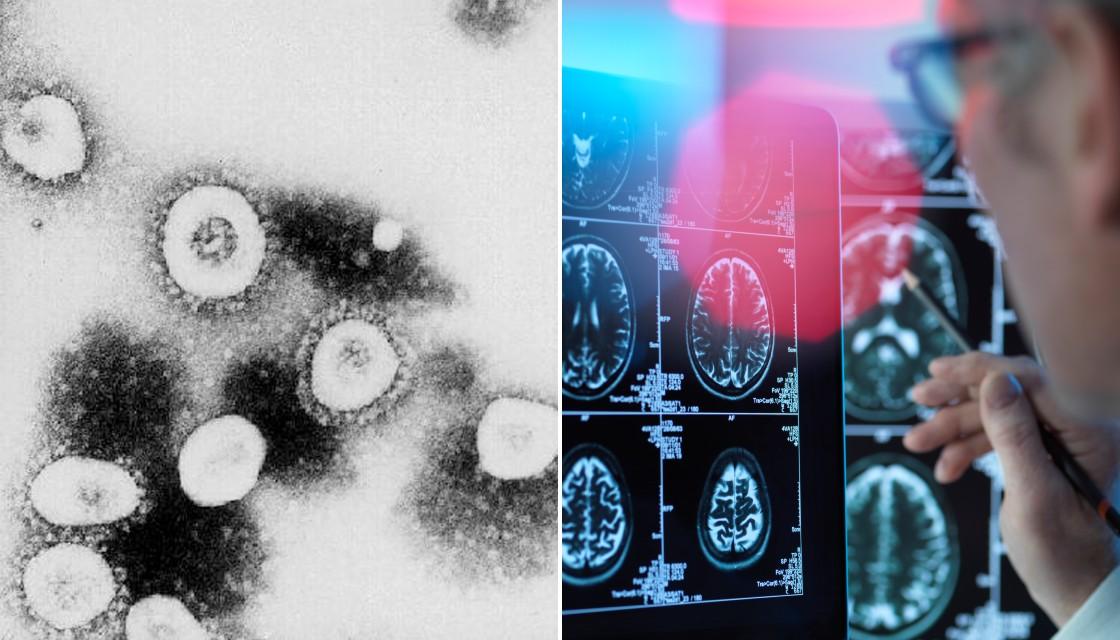
A new study has revealed COVID-19 can invade and "hijack" brain cells and suck up oxygen to kill others in some patients.
Despite COVID-19 mainly being a respiratory illness, recent studies have also found about half of patients report neurological symptoms including headaches, confusion, delirium.
Scientists from Yale University published a new study on Tuesday which investigates the effects of COVID-19 on the brain.
The study, which is yet to be peer-reviewed, found evidence that coronavirus can invade brain cells and "hijack" them to make copies of itself.
The virus also seems to suck up all of the oxygen nearby, starving adjacent cells to death.
But the researchers couldn't find any evidence of an immune response to stop the virus.
Lead researcher Dr Akiko Iwasaki told the New York Times it's like a "silent infection".
"This virus has a lot of evasion mechanisms," she said.
While these effects are considered to be rare, some people may be more susceptible due to their genetic background or other health conditions, the study said.
"If the brain does become infected, it could have a lethal consequence," Dr Iwasak said.
In the study researchers documented brain infection in brain tissue from a person who died of COVID-19, in a mouse, and in clusters of brain cells in a lab dish.
The virus was found to infect the brain cells through a protein on its surface called ACE2.
ACE2 appears throughout the body, particularly in the lungs which is likely why the virus targets the organ, the New York Times reported.
The scientists also looked at two sets of mice - one with the ACE2 receptor only in the brain, and the other with it only in the lungs.
When they were infected with COVID-19, the brain infected mice rapidly lost weight and died in six days, but the lung infected mice wasn't affected.
Dr Iwasaki said researchers should now investigate how common brain infection is among people with mild cases of COVID-19 and long-haulers (people with long term effects from COVID-19).


